Discover the science behind dental remineralization and explore safe, effective alternatives to fluoride—like nano-hydroxyapatite and CPP-ACP—for your child’s smile. Expert advice from a pediatric dentist you can trust.
As a pediatric dentist and a parent, I know how important it is to make informed, balanced decisions regarding your child’s health. Among the most frequent questions I hear is: “Is fluoride really necessary?” The answer, as with many things in medicine, is nuanced. This article explores fluoride and its scientifically backed alternatives—like nano-hydroxyapatite and casein phosphopeptide—to help you make confident, evidence-based choices for your family.
What Are Teeth Made of?
Our teeth are composed of three layers. The outermost layer is called enamel. This is the tooth’s protective shell. Tooth enamel is highly mineralized and is primarily composed of hydroxyapatite, a mineral form of calcium phosphate. It is the hardest biological material in the human body. The layer underneath the enamel is called dentin. It is less mineralized than enamel and surrounds the dental pulp which holds nerves and blood vessels.
What Is Dental Remineralization—and Why Does It Matter?
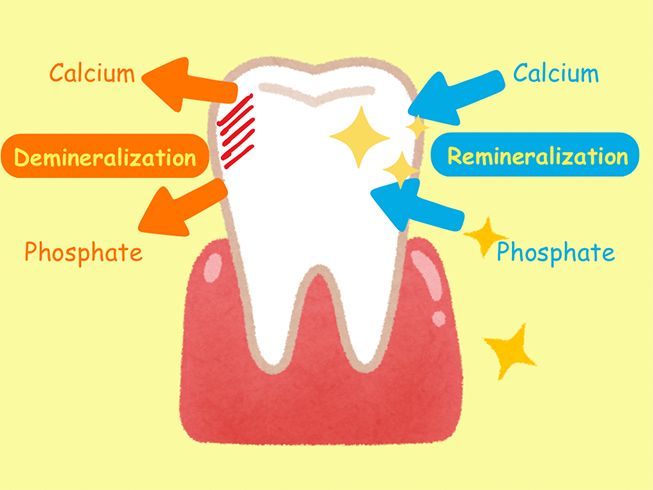
Our teeth are not static—they go through natural cycles of mineral loss (demineralization) and repair (remineralization) every day. These processes are influenced by what we eat, how often we brush, and the minerals present in our saliva and oral care products.
Remineralization is the process by which minerals, primarily calcium, and phosphate, are redeposited into enamel to repair early damage and keep teeth strong. In children, whose enamel is still developing and whose diets and habits may fluctuate, supporting remineralization is essential for preventing cavities and promoting long-term oral health.
Reference: Featherstone JDB. Dental caries: a dynamic disease process. Aust Dent J. 2008.
The Oral Microbiome
The mouth is a home to a vast array of microorganisms similar to those that reside in the gut. This intricate ecosystem is responsible for shifting the oral environment to one that favors either remineralization or demineralization. A healthy oral microbiome is predominately comprised of tooth-friendly organisms. While a microbiome that poses challenges to the dentition has elevated levels of acid-creating bacteria that can damage and erode enamel.
This organism’s balance is influenced by many factors. Some of which will tip the scale in favor of oral health and others that will do the opposite. Diet plays a big role in this balance; with highly processed foods and repetitive sugary snacks being at the forefront of factors that cause acid production in the mouth.
In contrast, healthy, whole foods have been shown to support dental health. Mineral-rich foods and foods rich in nitrate (such as leafy greens) are not only great for our bodies but also enhance our oral health.
Reference: Featherstone, J. D. B. (2004). The caries balance: The basis for caries management by risk assessment. Dental Clinics of North America, 53(1), 87–105.
The Oral PH
Oral PH refers to the acidity or alkalinity of the saliva and the oral environment. It is important to understand that the mouth is the beginning of the digestive tract. Digestion starts in the mouth and a reduction in PH levels is a natural outcome of this process. When PH levels are low in the mouth, demineralization will occur on the enamel surfaces.
However, it is transient and typically buffered within 30 minutes, when circumstances are favorable. A healthy mouth can easily recoup from this transient remineralization. In essence, enamel can heal by attracting minerals back into its superficial layers.
When PH levels stay low for extended periods of time, it becomes more challenging for this natural healing to occur. The balance tips in favor of demineralization and the enamel loses mineral content.
If this continues, superficial damage will occur on the tooth surface. Damage that has progressed into structural loss is commonly called a dental cavity. Common reasons for this to happen are frequent snacking and grazing on sugary or sticky foods that take a long time to clear the mouth.
CAMBRA
CAMBRA is an acronym for Caries Management By Risk Assessment. The purpose of this tool is to categorize individuals by their relative risk for developing dental caries, based on risk factors that include diet, oral hygiene, fluoride exposure, and past health history.
CAMBRA is a valuable resource in understanding how to promote oral health and well-being. It also allows the identification of factors or practices that should be avoided to support optimum oral health.
Reference: Featherstone, J. D. B., Doméjean, S., Jenson, L., Wolff, M., & Young, D. A. (2012).Caries Management by Risk Assessment (CAMBRA): An update for use in clinical practice.The Journal of the California Dental Association, 40(10), 852–857.
Fluoride: Still the Gold Standard?
Fluoride is the most studied and widely endorsed remineralizing agent in pediatric dentistry worldwide. However, newer data supports that the effects of fluoride are mostly due to a topical effect rather than a systemic one. Therefore, the question of the necessity of water fluoridation is currently a big topic of debate. Fluoride’s mechanism on teeth is threefold:
- It promotes remineralization of early enamel lesions.
- It inhibits demineralization by forming fluorapatite, which is more resistant to acid.
- It suppresses acid-producing bacteria like Streptococcus mutans.
Low-dose fluoride toothpaste and in-office fluoride varnish applications are supported by major health authorities, including the American Academy of Pediatric Dentistry (AAPD) and the American Dental Association (ADA).
That said, some parents—especially in health-aware communities—may express concern about fluoride exposure. It is important to differentiate between systemic ingestion (like in water fluoridation) and topical use, which is the foundation of pediatric fluoride therapy today. It is also important to understand that fluoride’s effects are dose-dependent. It is essential to consider the age and weight of a child to ensure that their overall exposure stays within safe amounts.
References:
AAPD Guideline on Fluoride Therapy.
Ten Cate JM. Contemporary perspective on the use of fluoride products. Br Dent J. 2013.
Understanding Parental Concerns About Fluoride
Fluoride hesitancy often stems from valid concerns about overexposure, fluorosis, or broader lifestyle choices centered around natural health. As providers, we always honor a parent’s desire to learn and advocate for their child’s well-being.
Mild fluorosis—characterized by faint white spots on teeth—can occur if young children swallow too much toothpaste. This is why we emphasize using a rice-sized smear of fluoride toothpaste for children under age 3, and a pea-sized amount for those 3 to 6, always under supervision.
The key is context and dosing. Just as we carefully dose medications for children, fluoride must be used thoughtfully. When used topically and in the right amount, it can help support stronger tooth structure and reduce the prevalence of dental caries.
Reference: Peckham S, Awofeso N. Water fluoridation: a critical review. Scientific World Journal. 2014.
Fluoride-Free? Let’s Talk Evidence-Based Alternatives
For families who prefer to avoid fluoride, there are clinically supported fluoride alternatives that offer real benefits. Here are the top options we use and recommend:
-
Nano-Hydroxyapatite (nHA): Nature-Inspired Enamel Repair
Nano-hydroxyapatite is a synthetic form of the mineral that makes up over 90% of tooth enamel. These ultra-small particles bond to the surface of the teeth, filling in microscopic pores and early lesions to rebuild and protect enamel.
- Biomimetic: It mimics natural tooth structure
- Non-toxic and biocompatible
- Effective at reducing sensitivity and improving surface smoothness
nHA is widely used in Japan and the EU and is growing in popularity here in the US. It is ideal for children with developing teeth, sensory sensitivities, or families who want a non-fluoride remineralizing option.
Link : Boka Fluoride Free Toothpaste Nano Hydroxyapatite
References:
- Huang S, et al. Remineralization potential of nano-hydroxyapatite. J Dent. 2009.
- Najibfard K, et al. A nano-hydroxyapatite dentifrice study. J Clin Dent. 2011.

Topical Oral Rinse with Fluoride
-
Casein Phosphopeptide-Amorphous Calcium Phosphate (CPP-ACP)
Derived from the protein casein in milk, CPP-ACP works by stabilizing and delivering bioavailable calcium and phosphate ions to the enamel surface. It is proven to remineralize white spot lesions and reduce caries in children and adolescents.
- Often recommended during orthodontic treatment
- Also available with fluoride for a synergistic effect (CPP-ACPF)
- Not suitable for patients with a milk protein allergy
Commonly marketed as MI Paste, this agent is well tolerated and backed by research.

Link: MIPaste
References:
- Reynolds EC. Casein phosphopeptide remineralization. J Dent Res. 1997.
- Cochrane NJ, et al. Clinical evaluation of CPP-ACP. Caries Res. 2008.
-
Xylitol: More Than a Sweetener
While not a remineralizing agent per se, xylitol is a natural sugar alcohol that is extracted from birch tree fibers. It reduces cavity-causing bacteria and enhances saliva flow, which supports natural remineralization. Xylitol gum or mints can be a valuable tool in caries prevention when used consistently.
We also like that these products offer an alternative to sugary treats for kids. We feel that offering a healthier option gets kids involved in their oral care rather than feeling that they must avoid sweets altogether.

Link: ZolliPops Sugar Free
Reference: Mäkinen KK. Sugar alcohols and caries. Int J Dent. 2010.
What We Recommend at Smiles:
In our pediatric dental practice, we take a personalized approach to remineralization based on each child’s:
- Age
- Caries risk
- Dietary habits
- Medical needs
- Family environment
For high-risk children, we often recommend the following during our dental visits:
- Fluoride varnish every 3–6 months
- Prescription-strength fluoride toothpaste or rinses for older kids
- nHA or CPP-ACP pastes for fluoride-free families
- Xylitol gum or mints for children able to chew safely
- Nutritional guidance to support the oral microbiome
- Education on oral hygiene practices
- Preventive measures to avoid dental caries
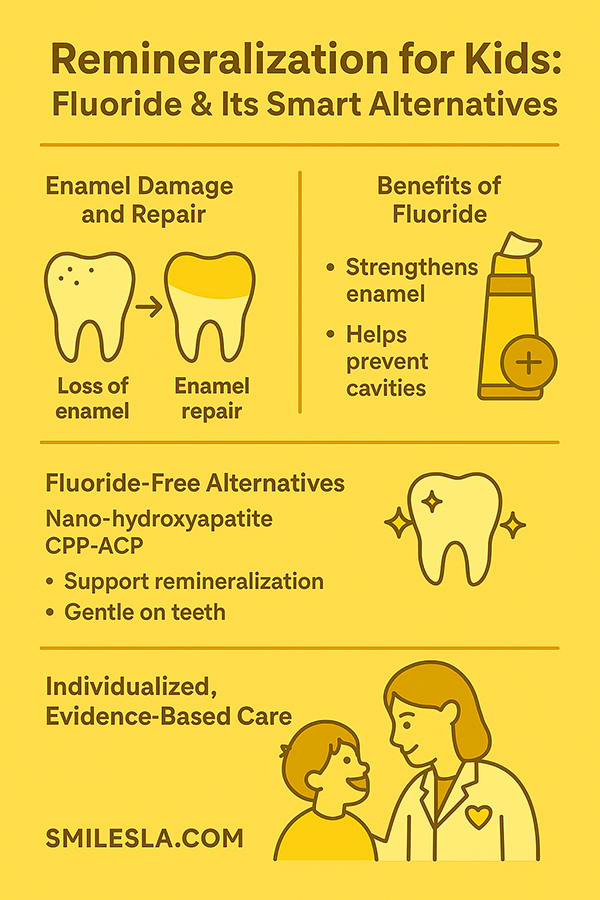
Empowering Parents: Science and Choice Can Coexist
We believe in educating, not pressuring. Our goal is to offer science-backed guidance while honoring parents’ instincts and preferences. Whether you choose fluoride, nHA, CPP-ACP, or a blend of these, your child can achieve excellent oral health with the right support and habits.
About the author, Dr. Reem:
Dr. Reem Kabbarah is a specialized pediatric dentist, mother, and educator who was recently featured in Spectrum News. In the article, she discussed the importance of fluoride in preventing cavities. Dr. Kabbarah emphasizes that while fluoride strengthens enamel, there are also safe fluoride-free alternatives for parents seeking options for their children’s dental care.
Spectrum News: Read the full article here
Final Thoughts: A Personalized Path to Stronger Smiles, Key Takeaways
Informed decisions create empowered parents. Fluoride is a proven tool in cavity prevention, but it is not the only option. Thanks to scientific advances, families now have more choices than ever when it comes to protecting their child’s smile—without compromising safety or integrity.
If you have questions, want product recommendations, or are curious about a customized remineralization plan for your child, we’re here to help. Our goal is to support your family’s values while providing the best possible care for your child’s dental future.
Q & A:
1- Is Fluoride necessary for toddlers?
Getting a toddler used to a consistent rhythm of oral hygiene is super important. A pleasantly tasting toothpaste is a great way to make brushing fun. Most toddler toothpastes are fluoride-free and labeled “safe to swallow”. For toddlers who have experienced early childhood caries, a comprehensive prevention will be set up. This plan can include a fluoride toothpaste option.
2- My child is young and can’t spit out his toothpaste, what should I do?
It is common for young children to swallow toothpaste. They don’t quite understand the concept of spitting or they really like the flavor and want to eat it!
We recommend a very small amount of paste (the size of a grain of rice). We also recommend that parents wipe out their toddler’s mouth with a wet washcloth after brushing to remove excess paste. This will help prevent the child from swallowing large amounts of toothpaste. For kids over the age of three, the amount of toothpaste can be increased to the size of a green pea.
3- My teenager won’t brush their teeth in the morning and wants to use mouth rinse instead. What can I do?
We love to educate teens on the importance of oral health. Once teenagers understand how certain habits can influence their oral well-being, they are more likely to commit to consistent and healthy practices. While mouth rinses can help remove oral plaque, they are not a substitute for good brushing with a toothbrush, manual or electric.
4- What kind of mouth rinse should my child use?
Mouth rinses help control harmful oral bacteria. However, many tend to be quite harsh and eradicate the good bacteria in the oral microbiome as well. Depending on the specifics of each child, we may or may not recommend using mouth rinses. Keep in mind that small children have yet to master the art of spitting so oral rinses are not recommended for kids under the age of 6.
5- What is tooth remineralization?
Remineralization is the process by which minerals are attracted back into the outer layer of enamel. This happens naturally once the PH level of our saliva is normalized after eating. Remineralization can also be enhanced by agents that promote a favorable environment that allows minerals to be present in the saliva and available for uptake by the enamel surfaces. These agents include natural substances like nitrate-rich foods and agents introduced into the saliva like fluoride, nano-hydroxyapatite (nHA), and Casein Phosphopeptide-Amorphous Calcium Phosphate.
6- What are the signs of tooth remineralization?
An incipient carious lesion (the very beginning of a cavity) looks like a white, chalky mark on the surface of the enamel. When examined, the surface feels rough and weak. When an area like this remineralizes, the enamel surface heals and hardens. The area may still show some chalkiness or discoloration but is considered sound enamel.
Some of the links in blog post may be affiliate links. This means that at no additional cost to you, I may earn a small commission if you make a purchase through these links. I only recommend products and services that I trust and believe will add value to my readers as pediatric dentist in Los Angeles.
Dr. Reem