Learn about the evolution of laser in pediatric dentistry, from early experiments to today’s anesthesia-free treatments. Modern laser technology delivers comfort, precision, and healing—transforming children’s dental experiences while promoting lifelong oral health through minimally invasive, advanced care.
As a pediatric dentist, I truly believe that the most important roll I play is to promote oral health and wellness for life. To me, that means honoring the magnificence of the human body and its amazing capacity to regenerate and heal. After spending years perfecting my skills in traditional dentistry, I never stopped searching for alternative pathways to promote oral health. When I was introduced to laser technology, I knew it would be game changer. Laser has offered me an instrument that is not only healing but is also artistic in its power. The technology has truly transformed the way I practice and serve the children that visit our office.
At Smiles Pediatric Dentistry & Orthodontics, we are proud to be part of the dental laser evolution. Our laser therapies bring healing, comfort, precision, and compassion to modern pediatric and teen dental care, often without the need for injections, numbness or drills.
Let’s explore this fascination technology and how it is shifting the way we are providing dental care.

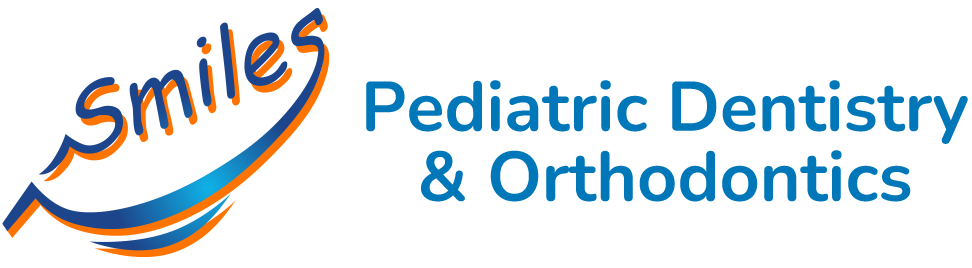
The Power’s in the Light:
Dental procedures are a lot for an adult to handle let alone a child, yet they are commonly underrated in complexity. In their truest nature, they are microsurgical procedures which have been traditionally performed with mechanial instruments.Laser innovations have transformed dental experiences from being tactile and jarring to smooth and flowing. The sensations that are experienced throughout the care are more comfortable and the treatment is minimally invasive when compared with traditional methods.
Laser does not “cut” tooth structure. It ablates it when the tooth absorbs the laser’s power. What is even more facinting is that lasers can also have a healing effect that promotes wellness.

Laser Throwback:
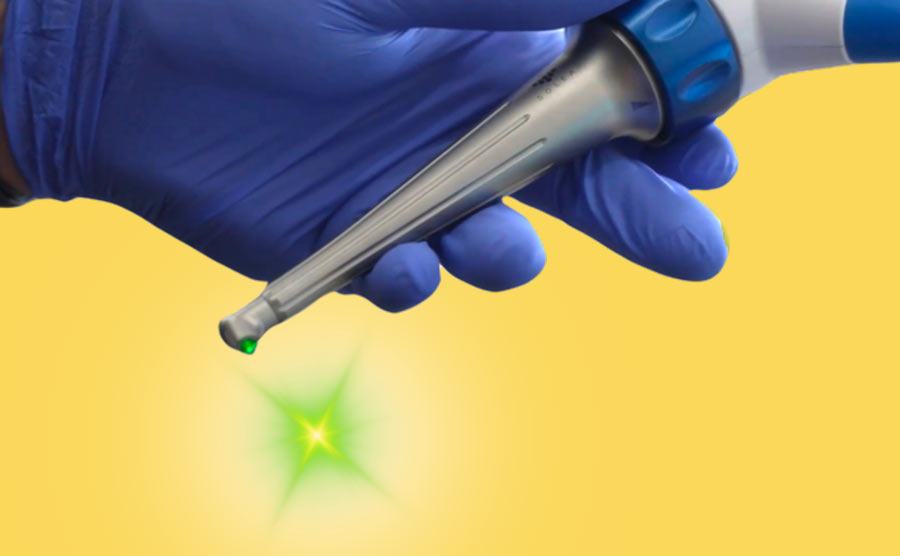
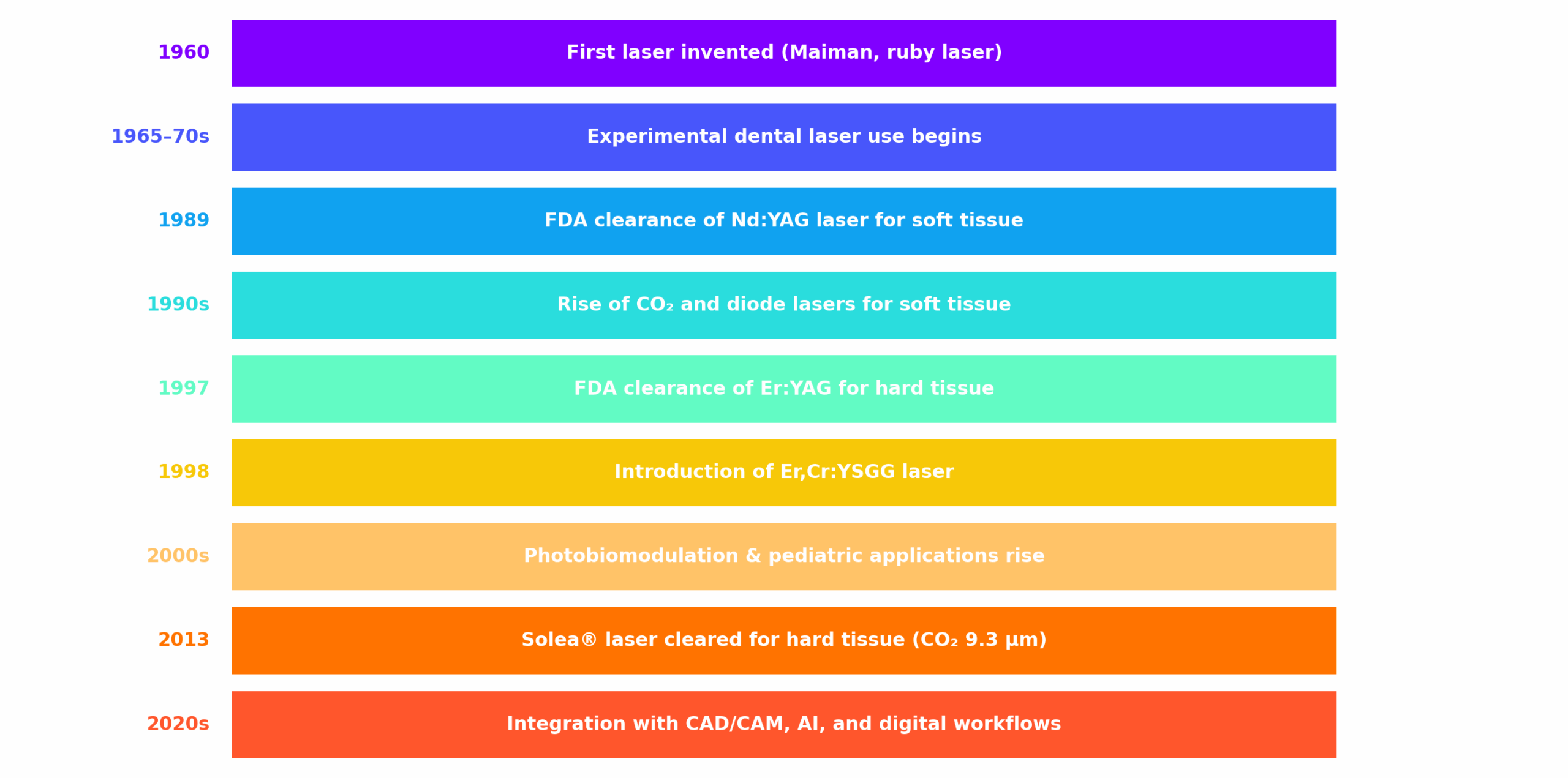
The concept of lasers began in theoretical physics. In 1917, Albert Einstein introduced the principle of stimulated emission, setting the stage for laser development. By 1960, Theodore Maiman built the first working laser using ruby crystal. This early technology was soon applied in medicine, with pediatric dentistry and laser dentistry exploring its potential by the late 1960s.
Albert Einstein by Oren Jack Turner (1947)
commons.wikimedia.org
The Early Days: Experimental Use in Dentistry
During the 1960s and 70s, researchers experimented with ruby and CO₂ lasers on teeth and gums. While promising, these first attempts were limited by thermal damage and lack of precision.
Stepping into the Clinic: FDA Approval and Soft Tissue Care
The first real clinical milestone came in 1989 when the FDA cleared the Nd:YAG laser for soft tissue dental use. In the 1990s, soft tissue lasers like CO₂ and diode lasers became popular for procedures like gingivectomy, frenectomy, and periodontal therapy, offering bloodless surgery and faster healing.
The Era of Hard Tissue Lasers
In 1997, a breakthrough came with the FDA’s clearance of the Er:YAG laser for hard tissue applications in enamel, dentin, and bone. The following year, the Er,Cr:YSGG laser debuted, combining versatility with precision. Dentists could now prep cavities and treat bone more gently than ever before.
Modern Laser Dentistry: Solea® and Beyond
In 2013, the Solea® laser was introduced. Solea offers CO₂ laser technology optimized for both soft and hard tissues. Its 9.3 µm wavelength made it possible to prep teeth without needles or drills. It is currently the latest laser option on the market that has the widest range of treatment options. In the 2020s, lasers became integral in cosmetic contouring, periodontal regeneration, and digital workflows with CAD/CAM and 3D printing.
Timeline Summary: Major Milestones in Laser Dentistry
How Can Lasers Have a Healing Effect In Dentistry?
The healing effects of lasers are not simply anecdotal. They are grounded in robust cellular biology, clinical research, and decades of technological refinement. Understanding how lasers facilitate healing requires a look at both the underlying science and their practical applications.
Biological Effects of Dental Lasers
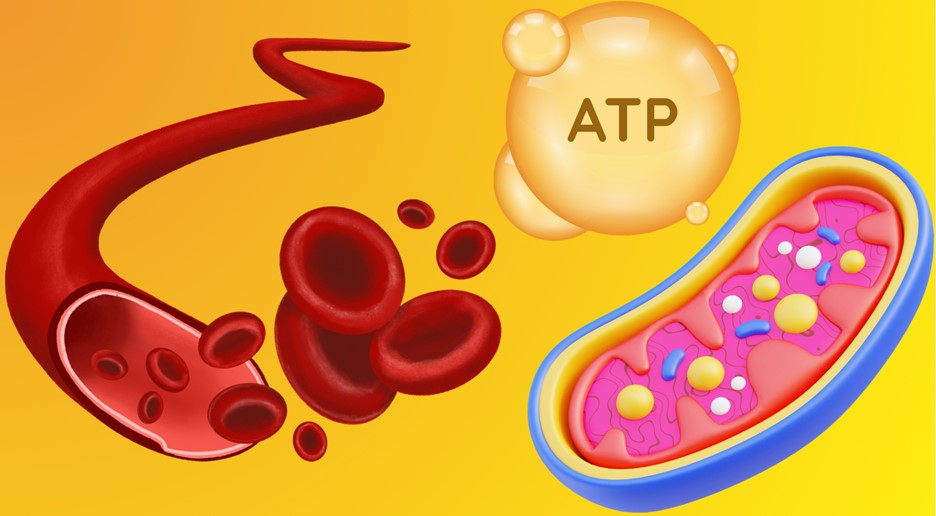
- Enhanced Cellular Energy and Repair
- ATP Boost: More ATP means cells can repair themselves faster and more efficiently.
- Fibroblast Proliferation: Fibroblasts, the cells responsible for producing collagen and extracellular matrix, are stimulated, leading to faster wound closure and tissue regeneration.
- Osteoblast and Osteoclast Activity: In bone, lasers can stimulate osteoblasts (bone-forming cells) and modulate osteoclasts (bone-resorbing cells), supporting bone remodeling and regeneration, crucial in orthodontics.
- Modulation of Inflammation
- Cytokine Regulation: PBM reduces the production of pro-inflammatory cytokines (such as IL-1, IL-6, TNF-alpha) and increases anti-inflammatory mediators.
- Reduced Swelling and Redness: This leads to less postoperative swelling, erythema, and discomfort.
- Faster Resolution of Inflammatory Lesions: Conditions like aphthous ulcers and herpetic lesions heal more quickly with laser therapy.
- Analgesic (Pain-Relieving) Effects
- Endorphin Release: Laser therapy can stimulate the release of endorphins, the body’s natural painkillers.
- Nerve Conduction Modulation: Lasers can temporarily block the transmission of pain signals along nerve fibers.
- Reduced Pressure on Nerves: By decreasing inflammation and edema, lasers relieve pressure on nerve endings, further reducing pain.
- Improved Vascularization and Circulation
- Angiogenesis: Lasers promote the formation of new capillaries in healing tissue, improving blood supply and nutrient delivery.
- Vasodilation: Enhanced blood flow accelerates the removal of waste products and supports tissue repair.
- Antimicrobial and Sterilizing Effects
- Bacterial Reduction: Certain laser wavelengths have bactericidal effects, reducing the microbial load in surgical sites and root canals.
- Sterilization of Wounds: This lowers the risk of postoperative infection and supports cleaner healing.
What is Photobiomodulation (PBM)?
Photobiomodulation (PBM), formerly known as low-level laser therapy (LLLT), is a non-thermal therapeutic technique that uses specific wavelengths of light (usually in the red to near-infrared spectrum, 630–1000 nm) to modulate cellular function. Unlike high-powered surgical lasers, PBM does not cut or ablate tissue. Instead, it delivers low-level energy that is absorbed by cellular chromophores, primarily cytochrome c oxidase in mitochondria, initiating a cascade of biological effects.
Clinical Effects in Dentistry:
- Pain Reduction: After orthodontic adjustments, extractions, or surgical procedures.
- Wound Healing: Faster recovery of soft tissue lesions, aphthous ulcers, and post-surgical sites.
- Reduction of Dentin Hypersensitivity: By modulating nerve response and promoting reparative dentin.
- Potential Acceleration of Orthodontic Tooth Movement: By stimulating bone remodeling (osteoblast and osteoclast activity), though evidence is variable.
The Gemini Laser Unit: Photobiomodulation In Action:
The Gemini 810 + 980 Diode Laser is a state-of-the-art, dual-wavelength soft tissue laser designed for both surgical and non-surgical dental applications. It is the first dual-wavelength diode laser available in the U.S., combining the benefits of two key wavelengths:
- 810 nm: Optimal absorption by melanin and hemoglobin, making it effective for cutting, coagulation, and hemostasis in pigmented soft tissues.
- 980 nm: Greater absorption by water, enhancing ablation and vaporization efficiency, and providing a different tissue interaction profile.
Key Features:
- Dual-Wavelength Operation: Use 810 nm, 980 nm, or both simultaneously for tailored clinical effects.
- Super-Pulsed Mode: Delivers high peak power in ultra-short pulses, minimizing collateral thermal damage and improving patient comfort.
- Versatility: Suitable for a wide range of soft tissue procedures and photobiomodulation applications.

The Healing Effects of The Solea CO₂ Laser Revolution:
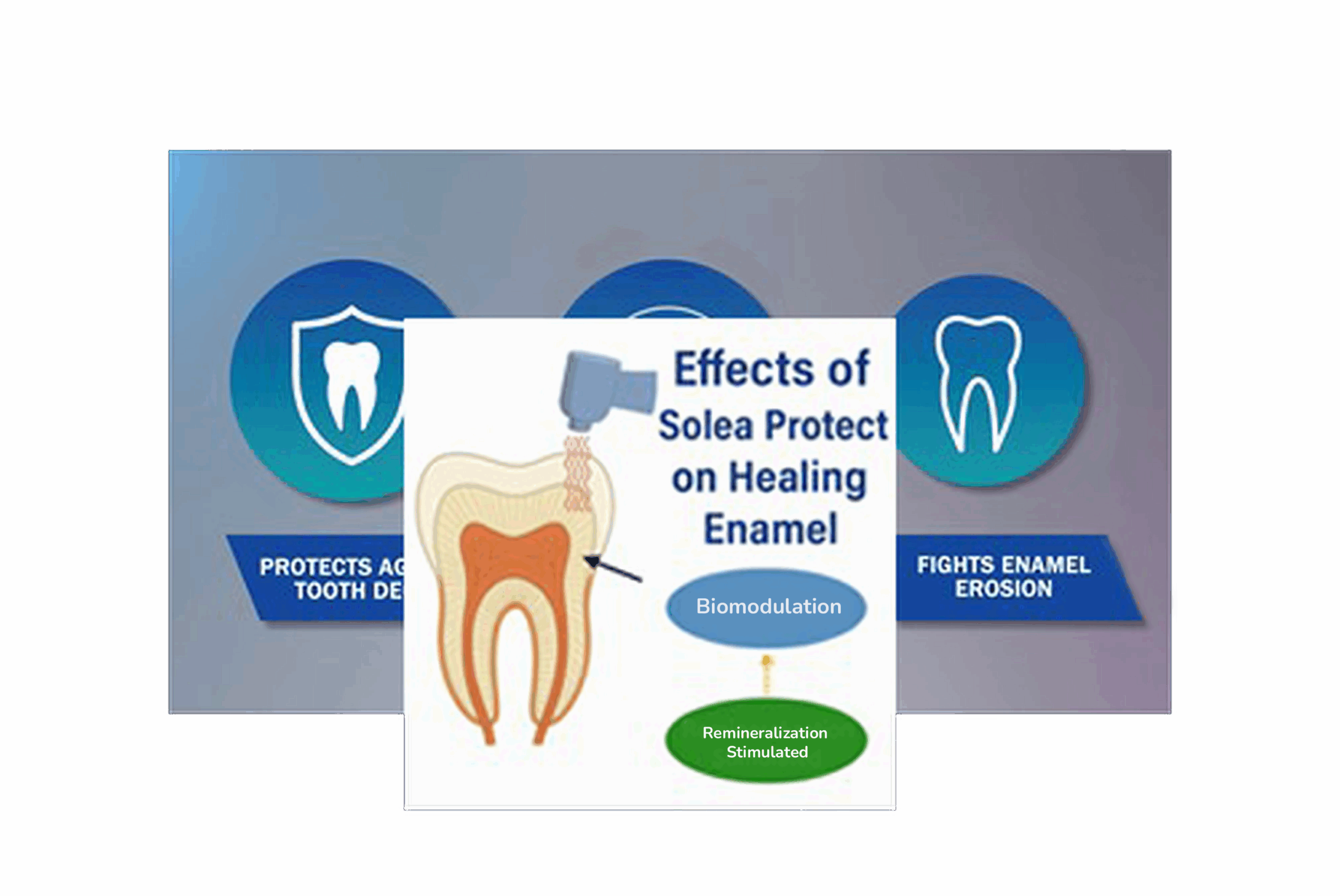
The Solea CO2 dental laser, when used with its “protect” handpiece, can thermally modify the enamel surfaces effectively “fusing” and “hardening” it. This makes enamel more resistant to acid attack and caries. The effect is achieved through controlled, sub-ablative laser energy that alters the crystal structure of enamel without removing tooth structure, and is clinically used for caries prevention, sealant preparation and reducing white spot lesions.

Scientific Basis: How CO₂ Lasers Modify Enamel
Wavelength and Enamel Absorption
-
The Solea CO₂ laser operates at 9.3 µm, a wavelength highly absorbed by hydroxyapatite, the primary mineral in enamel.
-
This absorption is far greater than with other dental lasers (e.g., Er:YAG, diode), making CO₂ lasers uniquely suited for precise, controlled interaction with hard tissues.
Thermal Modification, Not Ablation
-
When delivered at sub-ablative (non-cutting) energy settings, the laser gently heats the enamel surface.
-
This controlled heating does not vaporize or remove enamel, but instead induces a micro-melting and rapid re-solidification (recrystallization) of the outermost enamel layer.
Chemical and Structural Changes
-
The process drives out carbonate ions from the hydroxyapatite lattice.
-
Carbonate-rich hydroxyapatite is more acid-soluble; removing carbonate creates a purer, denser, and less acid-soluble crystal structure.
-
The result: increased microhardness and significantly improved resistance to acid demineralization, the fundamental process behind caries.
“Fusing and Hardening” Explained
-
“Fusing” refers to the partial melting and re-solidification of enamel crystals at the micro-scale.
-
“Hardening” reflects the measurable increase in surface microhardness and acid resistance.
-
These effects are well-documented in the scientific literature and are the basis for laser-based caries prevention protocols.
Clinical Applications and Benefits
A. Caries Prevention
-
Laser conditioning of enamel is especially valuable for high-risk patients, newly erupted molars, and pediatric populations.
-
Studies show a significant reduction in caries incidence on laser-treated surfaces compared to untreated controls.
B. Sealant Preparation
-
Pre-treating pits and fissures with the Solea laser before sealant placement:
-
Cleans and sterilizes the surface.
-
Increases sealant retention by creating a micro-roughened, acid-resistant surface.
-
Reduces microleakage and sealant failure rates.
-
C. White Spot Lesion Prevention (Orthodontics)
-
Laser treatment around orthodontic brackets can dramatically reduce the risk of white spot lesions, a common complication during fixed appliance therapy.
D. Hypersensitivity Management
-
By sealing exposed dentinal tubules, sub-ablative laser treatment can reduce sensitivity, especially in cervical areas.
E. Adjunct to Other Preventive Measures
-
Laser conditioning can be combined with fluoride application for synergistic effects, further enhancing enamel resistance.
Effects of Solea CO2 Laser on Oral Biofilm:
Oral biofilm (dental plaque) is a structured community of microorganisms embedded in a self-produced extracellular polymeric substance (EPS), adhering to teeth and soft tissues. Biofilm is the root cause of caries and periodontal disease, and its removal is a cornerstone of preventive and therapeutic dentistry. Bonded restorations require a clean surface to adhere to. Traditional mechanical debridement has its limitations, especially in young children.
Mechanisms of Solea’s Action on Oral Biofilm
- Rapid Water Absorption and Ablation
- Biofilm Composition: Up to 80% water, with bacteria, EPS, and host proteins.
- Laser-Biofilm Interaction: The Solea laser’s energy is absorbed by water molecules in the biofilm, causing instantaneous vaporization (ablation).
- Result: The biofilm is physically disrupted and removed from the surface, including from micro-irregularities and hard-to-reach areas.
- Bactericidal and Antimicrobial Effects
- Thermal Lethality: The rapid temperature rise denatures bacterial proteins, disrupts cell walls, and causes cell death.
- Spectrum of Action: Effective against a broad range of oral pathogens, including:
-
- Streptococcus mutans (caries)
- Porphyromonas gingivalis (periodontal disease)
- Fusobacterium nucleatum, Aggregatibacter actinomycetemcomitans, and others
- EPS Disruption: The laser breaks down the EPS matrix, which is the “slime layer” that protects bacteria from host defenses and antimicrobials.
- Prevention of Recolonization
- Surface Modification: Laser treatment can alter the surface energy and microtopography of enamel and dentin, making them less hospitable to new biofilm formation.
- Reduced Bacterial Adhesion: By disrupting the EPS and removing the initial colonizers, the laser impairs the ability of bacteria to reattach and form new biofilm.
- Clinical Applications and Advantages
- A. Caries and Restorative Dentistry
- Caries Removal: The laser can ablate carious tissue and associated biofilm, preparing a clean surface for adhesive restorations.
- Minimally Invasive: Reduces the need for rotary instruments, preserving healthy tooth structure and improving patient comfort.
- Dental Hygiene and Prophylaxis
- Adjunct to Routine Cleaning: The Solea laser can be used to remove biofilm from fissures, interproximal areas, and subgingival sites that are difficult to access with traditional instruments.
- Patient Comfort: No sharp instruments, less noise, and reduced vibration make the experience more pleasant, especially for
- Gingival Care and Health Maintenance
- Debridement: Solea can be used to debride and remove biofilm and inflamed tissue with minimal bleeding and discomfort.

How We Use Laser at Our Practice
At Smiles Pediatric Dentistry & Orthodontics, We use several laser units based on each child’s specific needs. Harnessing both CO2 and Diode (Gemini) laser theapy, we are able to offer soft and hard tissue laser theapy solutions in addition to the healing effects of photobiomodulation.
Here’s how we use Solea:
- Anesthesia-free cavity preparation for restorations
- Gentle procedures for children with sensory sensitivities or dental anxiety
- Efficient visits that reduce fear and increase cooperation
- Soft tissue procedures such as tongue-tie and lip-tie releases (frenulotomies/frenulectomies) with minimal trauma
- Surgical procedures for soft tissue like gingivectomy and gingivoplasty, biopsies
- Surgical procedure for hard tissues and impacted teeth
- Orthodontic tooth exposures involving soft tissue and bone
Here’s how we use Gemini:
- Soft tissue procedures: Gingivectomy and gingivoplasty, frenectomy (labial and lingual), hemostasis and coagulation, biopsy of soft tissue lesions
- Pain management for ulcers, cold sores and minor abrasions
- Photobiomodultion to promote healing post dental procedures and TMJ therapy
Where Science Meets Gentle Care
Laser dentistry is more than a leap in technology. It is a new philosophy of care, one that values comfort as much as clinical excellence. In my hands, the power of laser light has transformed the way I approach pediatric and teen dental care, and it continues to amaze me every day.
If you’re curious whether laser treatments are right for your child, we’re here to answer every question, and make every visit feel safe, modern, and full of smiles.
Schedule your child’s first dental visit today! Contact us here.